Key Facts
Over 5% of the world’s population – or 430 million people – require rehabilitation to address their ‘disabling’ hearing loss (432 million adults and 34 million children). It is estimated that by 2050 over 700 million people – or one in every ten people – will have disabling hearing loss.
‘Disabling’ hearing loss refers to hearing loss greater than 35 decibels (dB) in the better hearing ear. Nearly 80% of people with disabling hearing loss live in low- and middle-income countries. The prevalence of hearing loss increases with age, among those older than 60 years, over 25% are affected by disabling hearing loss.
Hearing loss and deafness
A person who is not able to hear as well as someone with normal hearing – hearing thresholds of 20 dB or better in both ears – is said to have hearing loss. Hearing loss may be mild, moderate, severe, or profound. It can affect one ear or both ears, and leads to difficulty in hearing conversational speech or loud sounds.
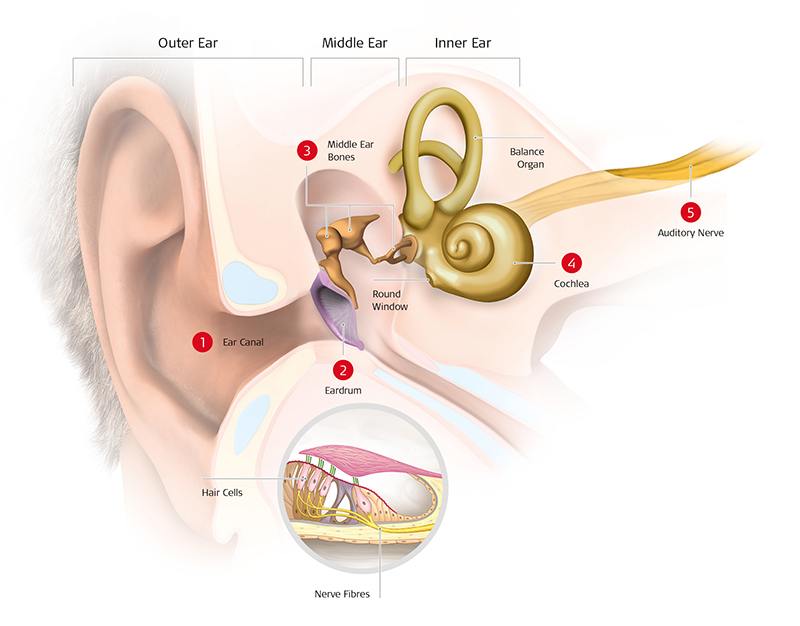
'Hard of hearing' refers to people with hearing loss ranging from mild to severe. People who are hard of hearing usually communicate through spoken language and can benefit from hearing aids, cochlear implants, and other assistive devices as well as captioning.
'Deaf' people mostly have profound hearing loss, which implies very little or no hearing. They often use sign language for communication.
Causes of hearing loss and deafness
Although these factors can be encountered at different periods across the life span, individuals are most susceptible to their effects during critical periods in life.
Prenatal Period
- Genetic factors - Include hereditary and non-hereditary hearing loss
- Intrauterine infections – such as rubella and cytomegalovirus infection
Perinatal period
- Birth asphyxia (a lack of oxygen at the time of birth
- Hyperbilirubinemia (severe jaundice in the neonatal period)
- Low-birth weight
- Other perinatal morbidities and their management
Childhood and adolescence
- Chronic ear infections (chronic suppurative otitis media)
- Collection of fluid in the ear (chronic nonsuppurative otitis media)
- Meningitis and other infections
Adulthood and older age
- Chronic diseases
- Smoking
- Otosclerosis
- Age-related sensorineural degeneration
- Sudden sensorineural hearing loss
Factors across the life span
- Cerumen impaction (impacted ear wax)
- Trauma to the ear or head
- Loud noise/loud sounds
- Ototoxic medicines
- Work related ototoxic chemicals
- Nutritional deficiencies
- Viral infections and other ear conditions
- Delayed onset or progressive genetic hearing loss
The impact of unaddressed hearing loss
When unaddressed, hearing loss impacts many aspects of life at individual level:
Communication and speech
Cognition
Education and Employment: In developing countries, children with hearing loss and deafness often do not receive schooling. Adults with hearing loss also have a much higher unemployment rate. Among those who are employed, a higher percentage of people with hearing loss are in the lower grades of employment compared with the general workforce.
Social isolation, loneliness and stigma
Impact on society and economy
Years Lived with Disability (YDLs) and Disability Adjusted Life Years (DALYs)
WHO estimates that unaddressed hearing loss poses an annual global cost of US$ 980 billion. This includes health sector costs (excluding the cost of hearing devices), costs of educational support, loss of productivity, and societal costs. 57% of these costs are attributed to low- and middle-income countries.
Prevention
Many of the causes that lead to hearing loss can be avoided through public health strategies and clinical interventions implemented across the life course.
Prevention of hearing loss is essential throughout the life course – from prenatal and perinatal periods to older age. In children, nearly 60% of hearing loss is due to avoidable causes that can be prevented through implementation of public health measures. Likewise, in adults, most common causes of hearing loss, such as exposure to loud sounds and ototoxic medicines, are preventable.
Effective strategies for reducing hearing loss at different stages of the life course include:
- immunization;
- good maternal and childcare practices;
- genetic counselling;
- identification and management of common ear conditions;
- occupational hearing conservation programmes for noise and chemical exposure;
- safe listening strategies for the reduction of exposure to loud sounds in recreational settings; and
- rational use of medicines to prevent ototoxic hearing loss.
Identification and management
- Early identification of hearing loss and ear diseases is key to effective management.
- This requires systematic screening for detection of hearing loss and related ear diseases in those who are most at risk. This includes:
- Newborn babies and infants
- Pre-school and school-age children
- People exposed to noise or chemicals at work
- People receiving ototoxic medicines
- Older adults
- Hearing assessment and ear examination can be conducted in clinical and community settings. Tools such as the WHO “hearWHO” app and other technology-based solutions make it possible to screen for ear diseases and hearing loss with limited training and resources.
- Once hearing loss is identified, it is essential that it is addressed as early as possible and in an appropriate manner, to mitigate any adverse impact.
- Measures available to rehabilitate people with hearing loss include:
- the use of hearing technologies, such as hearing aids, cochlear implants and middle ear implants;
- the use of sign language and other means of sensory substitution,such as speech reading, use of print on palm or Tadoma, signed communication; and
- rehabilitative therapy to enhance perceptive skills and develop communication and linguistic abilities.
- The use of hearing assistive technology, and services such as frequency modulation and loop systems, alerting devices, telecommunication devices,captioning services and sign language interpretation, can further improve access to communication and education for people with hearing loss.
WHO response
WHO’s work on ear and hearing care is to promote integrated people-centred ear and hearing care (IPC-EHHC).
WHO’s work is guided by the recommendations of the WHO World report on hearing (2021) and the World Health Assembly resolution on prevention of deafness and hearing loss.
WHO’s work includes:
- guide, assist and support Member States to increase awareness on EHC issues;
- facilitate data generation and dissemination of ear and hearing care related data and information;
- providing technical resources and guidance to facilitate planning and health systems capacity building for ear and hearing care;
- supporting heath workforce training in ear and hearing care;
- promoting safe listening to reduce the risk of recreational noise-induced hearing loss through the WHO Make Listening Safe initiative;
- observing and promoting World Hearing Day as an annual advocacy event;
- building partnerships to develop strong hearing care programmes, including initiatives for affordable hearing aids, cochlear implants and services;
- Advocating for ear and hearing care through the World Hearing Forum.
